
Click the link below the picture
.
By the time Maggie May, an Arkansas resident in her 30s, was admitted to a psychiatric clinic in 2024, she had been struggling for years with atypical anorexia nervosa, an eating disorder that leads to severe food restriction and profound disturbances in body image. (Her name has been changed for privacy.) She had already tried traditional interventions with a psychotherapist and a dietitian, but they had failed to improve her condition. So when May heard about a trial of a new and unconventional therapy, she jumped at the opportunity.
The treatment was unusual in that, alongside talk therapy, May underwent several sessions in a sensory-deprivation chamber: a dark, soundproof room where she floated in a shallow pool of water heated to match the temperature of her skin and saturated with Epsom salts to make her more buoyant. The goal was to blunt May’s external senses, enabling her to feel from within—focusing on the steady thudding of her heart, the gentle flow of air in and out of her lungs, and other internal bodily signals.
The ability to connect with the body’s inner signals is called interoception. Some people are better at it than others, and one’s aptitude for it may change. Life events can also bolster or damage a person’s interoceptive skills. Sahib Khalsa, a psychiatrist and neuroscientist at the University of California, Los Angeles, and his colleagues think a disrupted interoception system might be one of the driving forces behind anorexia nervosa. So they decided to repurpose a decades-old therapy called flotation-REST (for “reduced environmental stimulation therapy”) and launched a trial with it in 2018. They hypothesized that in people with anorexia and some other disorders, an underreliance on internal signals may lead to an overreliance on external ones, such as how one looks in the mirror, that ultimately causes distorted body image, one of the key factors underlying these conditions. “When they’re in the float environment, they experience internal signals more strongly,” Khalsa says. “And having that experience may then confer a different understanding of the brain-body relationship that they have.”
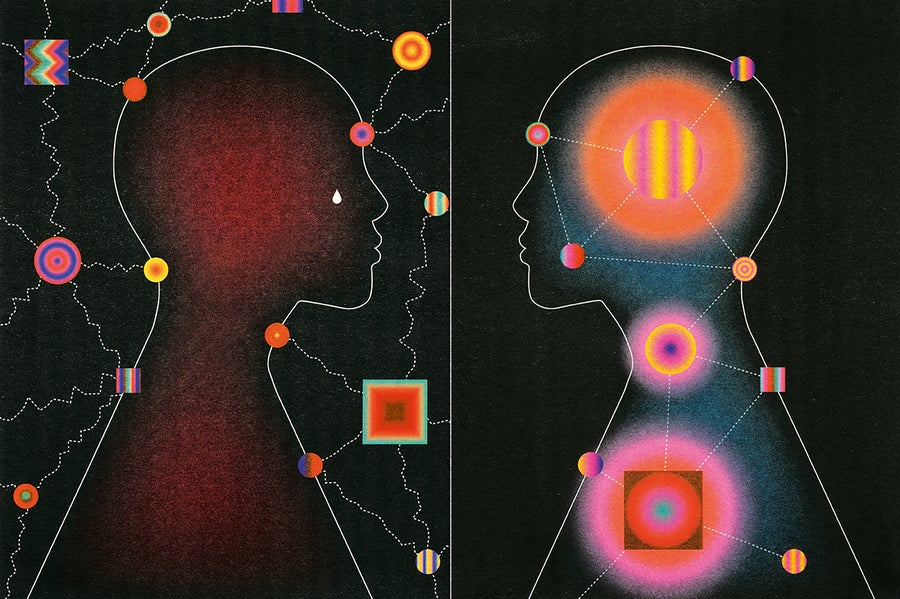
Studies have implicated problems with this inner sense in a wide variety of conditions, including anxiety disorders, post-traumatic stress disorder, and borderline personality disorder. Some researchers and clinicians now think that problems in interoception might contribute to many mental illnesses. Alongside this research, which itself is complicated by challenges in testing design and by a less than clear understanding of interoception, other groups are also developing therapies that aim to target this inner sense and boost psychological well-being.
This work is circling in on a central message: the body and mind are inextricably intertwined. “We have always thought about [mental health conditions] as being in the brain or the mind,” says Camilla Nord, a professor of cognitive neuroscience at the University of Cambridge. But clinicians have long noted that people with mental illness frequently report physical symptoms such as abnormalities in heartbeats, breathing, and appetite, she adds.
The idea that the body can influence the mind dates back centuries. In the 1800s, two psychologists on opposite ends of the globe independently proposed a then novel idea: emotions are the result of bodily reactions to a specific event. Called the James-Lange theory after its founders, American psychologist William James and Danish doctor Carl Lange, this view ran counter to the long-dominant belief that emotions were the cause, not a consequence, of corresponding physiological changes.
Although this notion has garnered critics, it inspired a slew of studies. The 1980s saw a surge of interest in the role of physiological signals in panic disorders. Researchers discovered that they could bring on panic attacks by asking people to inhale carbon dioxide–enriched air, which can increase breathing rates, or by injecting them with isoproterenol, a drug that increases heart rate.
Breathing rate can affect how someone perceives the intensity and unpleasantness of pain.
These findings led some psychologists to suggest that physical sensations were the primary trigger of panic attacks. In the early 1990s, Anke Ehlers, a psychologist then at the University of Göttingen in Germany, and her team examined dozens of people with panic disorders and reported that these patients were better able to perceive their heartbeats than healthy individuals—and that this greater awareness was linked to more severe symptoms. On top of that, a small, preliminary study by Ehlers of 17 patients revealed that those who were more skilled at this task were more likely to relapse and start having panic attacks again. These observations hinted at a two-way dynamic: not only could physical sensations within the body cause psychological effects, but the ability to perceive and interpret those signals—in other words, one’s interoceptive ability—could have a profound influence on mental health.
Over the years, a growing body of evidence has indicated that interoception plays an important role in shaping both emotions and psychological health. A large chunk of this work has focused on the heart. With every heartbeat, blood rushes into the arteries and triggers sensors known as baroreceptors, which shoot off messages to the brain conveying information about how strongly and rapidly the heart is beating.
In one pivotal 2014 study, Hugo Critchley, a neuropsychiatrist at Brighton and Sussex Medical School in England, and his team reported that this process can affect a person’s sensitivity to fear. By monitoring volunteers’ heartbeats while they viewed fearful or neutral faces, they found that people detected fearful faces more easily and judged them as more intense when their heart was pumping out blood than when it was relaxing and refilling. But participants with higher levels of anxiety often perceived fear even when their hearts relaxed.
Researchers have also demonstrated that bodily signals such as breathing patterns and gut rhythms can influence emotional reactions. People are quicker to react to fearful faces while breathing in than while breathing out, and breathing rate can affect how someone perceives the intensity and unpleasantness of pain.In more recent work, some neuroscientists have turned their attention to the gastrointestinal system. In 2021, Nord and her colleagues discovered that people given a dose of an antinausea drug that affects gut rhythms—processes within the stomach that help digestion—were less likely to look away from pictures of feces than they normally would have been. These disgust-related visceral signals, Nord speculates, may be relevant to eating disorders. “It’s possible that some of these signals contribute to feeling aversion to signals of satiety, making satiety very uncomfortable, a feeling you don’t want to feel,” she says.
.
 DTAN Studio
DTAN Studio
.
.
Click the link below for the complete article:
.
__________________________________________
Leave a comment