
Click the link below the picture
.
Recent headlines warning of concerns such as heart risks or danger to teenagers have put a new spotlight on a diet trend that has long been the popular epitome of a healthy lifestyle: intermittent fasting. “Intermittent fasting’s image has been deeply tarnished—and quite rightly so,” says Stefan Kabisch, a physician at the endocrinology and metabolic medicine department at Charité–University Medicine Berlin. “The hype was never really backed up by good data in humans.”
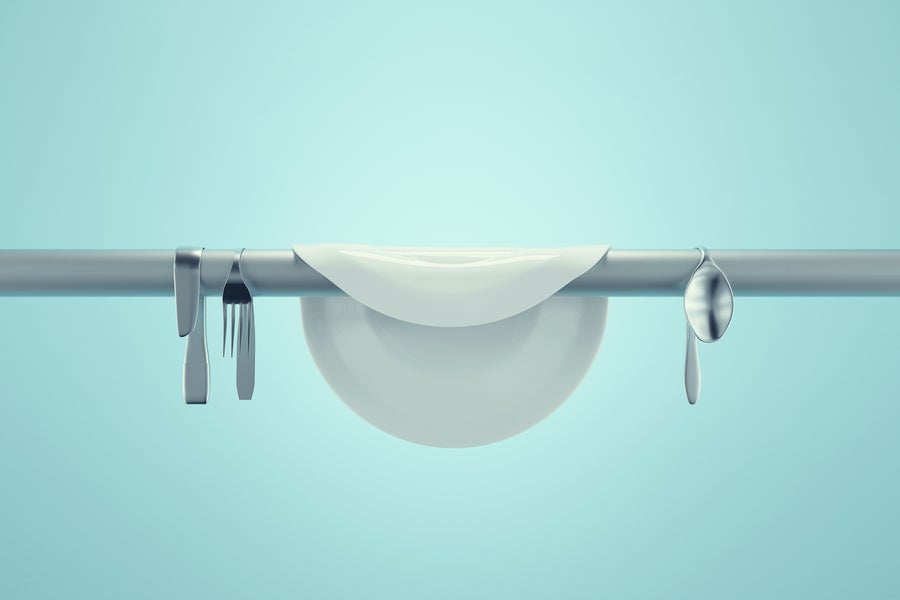
Advocates have claimed that temporarily abstaining from food for long stretches of the day can improve health and longevity. In the most common fasting schedule, people don’t eat for 16 hours—often skipping breakfast or dinner—and make up for it in the remaining eight hours (the so-called 16:8 method). Some people may severely limit food intake every other day (alternate-day fasting) or take a fasting day twice a week (the 5:2 method).
The effects of such practices can be difficult to study. “The main problem with randomized controlled trials on intermittent fasting is that there are so many variations,” Kabisch explains. “The data is therefore very heterogeneous, which makes it difficult to assess effects.”
Why Take Long Breaks from Eating?
Modern society has given way to lifestyles that encourage overeating, says Tinh-Hai Collet, a diabetologist and a professor at the Geneva University Hospitals. “This promotes obesity and diabetes.” Experts have called diabetes a global epidemic. Approximately 590 million people worldwide have diabetes, according to the latest 2025 reports from the International Diabetes Federation, and more than 90 percent of them have type 2, often called adult-onset diabetes.
One of the main issues in type 2 diabetes is that those who are affected absorb more energy than they use. A hallmark of the disease is insulin resistance, in which cells no longer effectively respond to the hormone insulin. This means cells take in less sugar from the blood, and blood sugar levels rise. “Intermittent fasting almost always improves the cells’ response to insulin,” says Stephan Herzig, a professor at the Technical University of Munich and head of the Helmholtz Diabetes Center at Helmholtz Munich. “As a result, the concentrations of sugar, fats, and cholesterol in the blood also fall.” A 2023 study, led by Mark Ezpeleta of the University of Illinois Chicago, suggests that alternate-day fasting—especially when combined with exercise—also mitigates fatty liver disease, in which fat builds up on in the liver, unrelated to alcohol consumption.
A closer look at the research, however, shows such statements may not be as clear-cut as they are often presented to be. For example, the researchers on the 2023 liver fat study compared volunteer groups that underwent different eating and exercise schedules: alternating days between a reduced calorie intake and an unrestricted diet; only completing an exercise program; combining the fasting schedule with exercising; or not undergoing any intervention. The group that fasted and exercised at the same time saw the best results. Yet there was no comparison group in which people didn’t alternate days but still had the same calorie intake as the fasting participants. “This is an unfair comparison,” Kabisch says. And similar gaps in study design “run through the entire literature on the subject.”
Two meta-analyses of people with diabetes or obesity concluded that intermittent fasting had a positive effect on weight, blood sugar, blood pressure, and blood lipids (triglycerides). “In most of the underlying primary studies, however, the fasting subjects were compared with people who did not change their diet,” Kabisch says. As a result, the subjects in the intervention groups lost weight—but, logically, the control groups did not, because the researchers didn’t apply any calorie restrictions. “You only see strong effects of intermittent fasting compared to people who were not given any diet or exercise guidelines,” Kabisch explains. “But as soon as you compare it with equivalent calorie reduction, the benefits of intermittent fasting disappear.”
And the supposed improvement in insulin resistance is also not always demonstrable. In another meta-analysis, no effects were found in this regard. In other studies, the improvements were small.
.
 Allvisionn/Getty Images
Allvisionn/Getty Images
.
.
Click the link below for the complete article:
.
__________________________________________
Leave a comment