
Click the link below the picture
.
Scientists announced this week that they have managed to keep a genetically modified pig lung alive inside a human body—although briefly—for the first time. The lung survived for nine days, marking what some researchers say is an early step toward a major, long-hoped-for medical breakthrough. But others note that the road ahead is still a lengthy one.
With available human organs constantly filling only a tiny fraction of transplant demand, scientists have been trying for decades to turn pigs into lifesaving donors. Many pig organs are close in size and structure to those of humans, and pigs are prolific breeders that are relatively easy to raise in a pathogen-free environment. Researchers have successfully transplanted pig kidneys, livers, and hearts into humans, but lungs have remained a daunting challenge because of their complex physiology.
For one thing, lungs contain many blood vessels and white blood cells called macrophages, which surround and kill bacteria and viruses. These cells rapidly produce immune responses—but they also tend to trigger rapid and potentially lethal inflammation when surgeons restore blood flow after reducing it during transplant surgery. Because of such complexity, “we knew lungs would be the last organ that will get into the clinic,” says Muhammad Mohiuddin, a surgeon and president of the International Xenotransplantation Association, who conducted the first pig-to-human heart transplantation in 2022 but was not involved with the new experiment. And although it “is a great achievement” for the field, “we have to be cautiously optimistic” because this is just an early foray into understanding this extremely difficult procedure.
A team of scientists at China’s Guangzhou Medical University transplanted the pig lung into the body of a 39-year-old recipient who had already been declared brain-dead. The researchers used the gene-editing technique CRISPR to alter three pig genes that are naturally targeted by human antibodies. They also added three human genes to help prevent rejection. From the resulting genetically modified pig, they transplanted the left lung into the recipient, whose body was kept on life support, to observe how the organ functioned and how the human immune system responded. They also administered immunosuppressants to help prevent rejection.
The transplanted lung remained functional for nine days and was not immediately rejected by the human body. The scientists did report signs of lung tissue damage—produced by the lack of oxygen during the transplantation—one day after surgery, however. And the immune system showed the first signs of antibody-mediated rejection on days three and six. The experiment was terminated on day nine at the request of the recipient’s family.
In the study, which was published in Nature Medicine this week, the authors said that the process needs significant improvements, such as optimizing the pig’s genetic modifications and the immunosuppressive drugs used to avoid long-term rejection of the organ. None of the authors responded to Scientific American’s interview requests.“I don’t think blindly adding more knockouts and transgenes is the solution,” says Columbia University immunologist Megan Sykes, referring to genetic changes to the donor pig. If scientists take that approach, she adds, each modification should be tested separately by transplanting the pig organs into a baboon—a primate that is often used as a prehuman test stop for transplants. Sykes was not involved with the surgery and has focused on pig-to-baboon experiments to establish a recipient’s tolerance of transplanted lungs “I think tolerance, as well as better control of innate immunity, is going to be essential for the success,” she says.
.
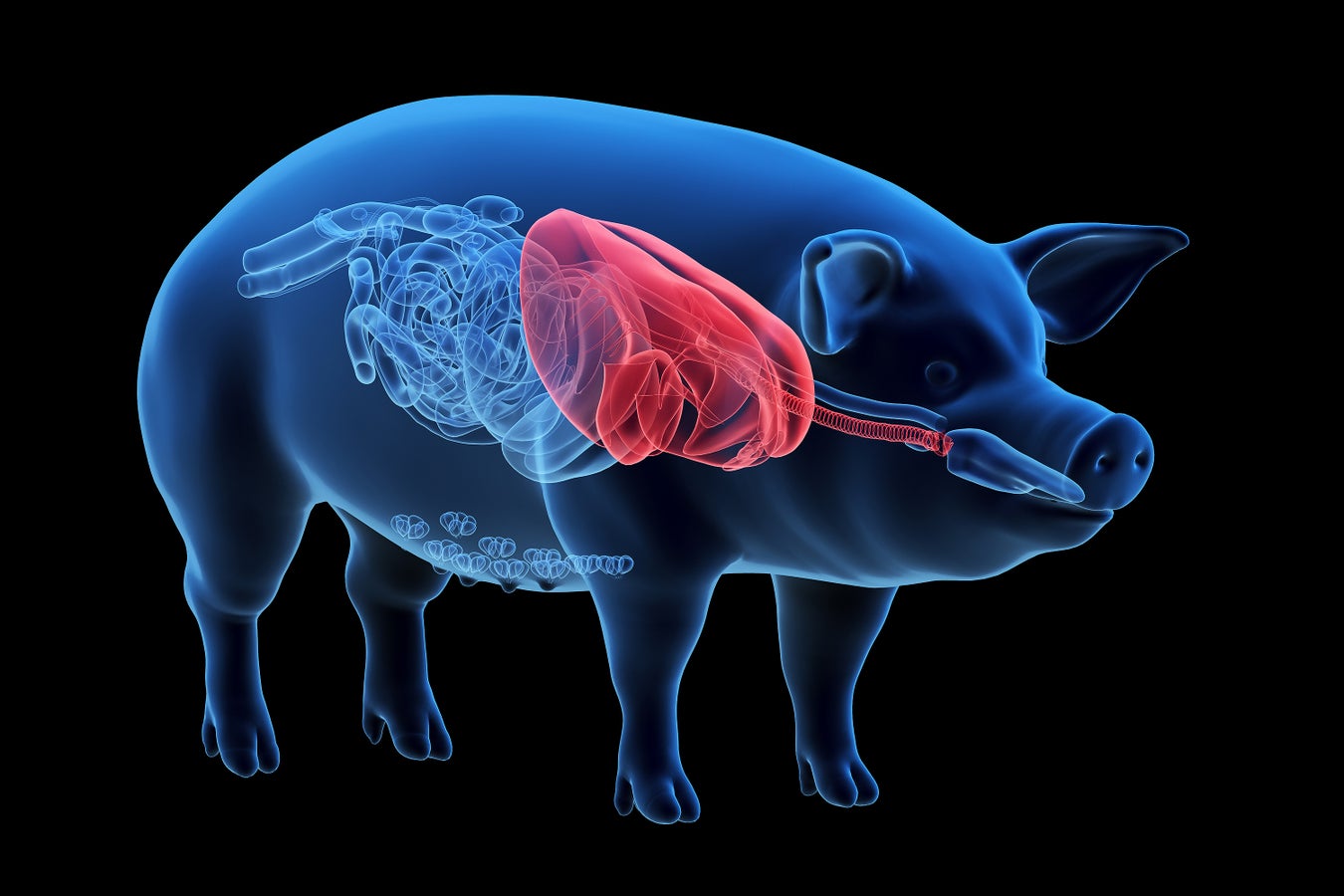
Illustration of pig lungs. Ebastian Kaulitzki/Science Source
.
.
Click the link below for the complete article:
.
__________________________________________
Leave a comment